As hospitals across the country will undoubtedly continue to see an increase in coronavirus patients, many are wondering how prepared the healthcare facilities in their region are for the influx.
New data released by the Harvard Global Health Institute (HGHI) breaks down which regions could be especially overwhelmed. Dr. Ashish Jha, director of HGHI, said “vast communities in America are not prepared to take care of the COVID-19 patients showing up.” A fifth of adults who are infected will need to be hospitalized, according to the data.
Researchers say some regions would have the capacity to handle the surge without adding new beds or displacing other patients but many will not.
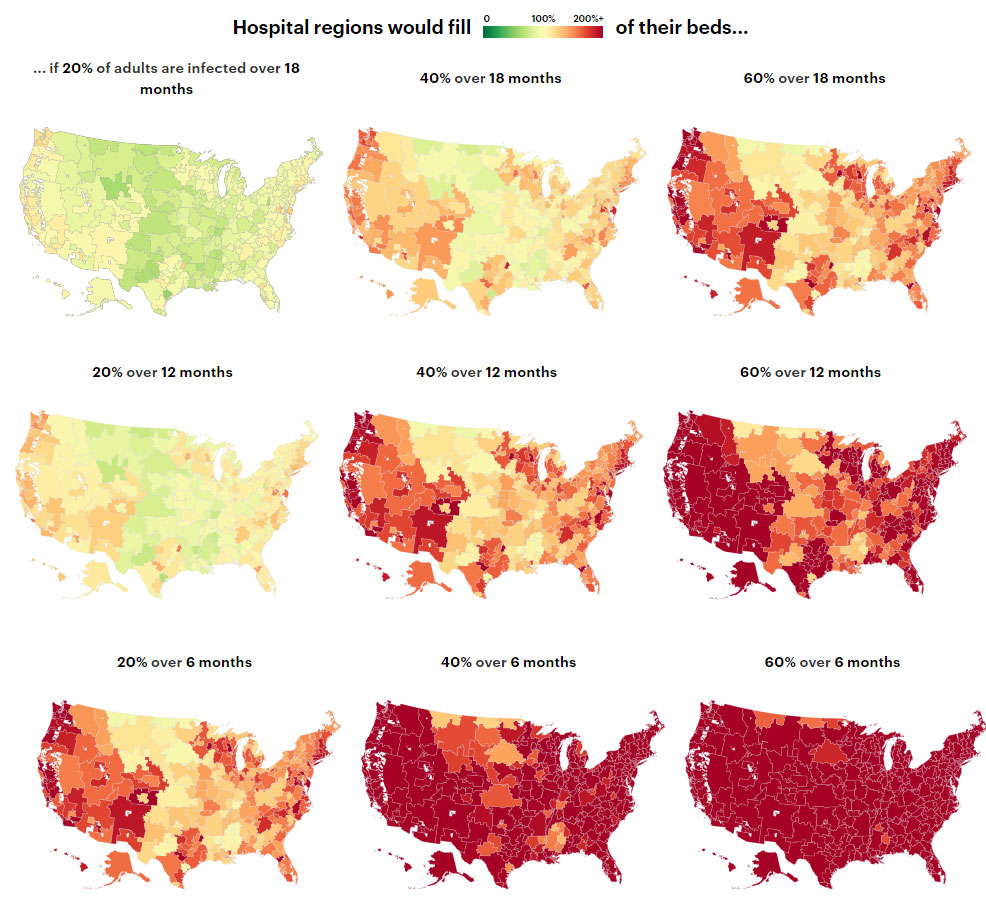
Jha and his team selected various percentages of infected Americans and modeled hospital capacity throughout the country for each percentage over three time periods — six months, 12 months and 18 months. The various scenarios articulate how Americans can “flatten the curve” through social measures to ensure hospitals have a greater capacity to care for COVID-19 patients, according to The Verge.
“The way to permanently stop new cases from setting off long chains of transmission is to have each case infect considerably less than one case on average,” said Dr. Marc Lipsitch, head of the Harvard T.H. Chan School of Public Health’s Center for Communicable Disease Dynamics. “The numbers will go down. There will still be little outbreaks, but not big ones.”
HGHI launched its estimates in collaboration with several organizations, including ProPublica, a non-profit newsroom that investigates abuses of power. ProPublica mapped out HGHI’s data into nine different scenarios.
What Are the Results of Best- and Worst-Case Scenarios?
Clearly, data shows it is ideal for the infection to spread over a longer period of time. Under the researchers’ best-case scenario, Americans will act quickly to slow the spread of the virus and “flatten the curve” through social distancing, and the infection rate among adults will remain at 20% — less than twice the number of Americans who get the flu every year.
Even in a best-case scenario, with coronavirus cases spread out over 18 months, American hospital beds would be 95% full. However, epidemiologists say the 20% estimate is conservative based on the infection rates of prior pandemics, according to ProPublica.
In comparison, the 2009 H1N1 swine flu pandemic infected approximately 60 million Americans over a year with no efforts of social distancing or containment made. However, current data suggests coronavirus is more contagious than the swine flu.
In a moderate scenario, where 40% of the adult population would contract COVID-19 over the course of a year, 98.9 million Americans would develop the disease, though many would have mild or no symptoms and will not have their diagnoses confirmed by testing. If that estimate holds true, nearly 5% of those infected would become critically ill from the virus and would need intensive care.
In other scenarios where the virus spreads faster or infects more citizens, hospitals would be forced to expand capacity, limit elective surgeries, or make life-and-death decisions about care — something that has already happened in the hardest-hit regions in Italy. Some doctors were directed to only treat patients “deemed worthy of intensive care” and to make decisions based on “distributive justice,” according to The Independent.
In the researchers’ worst-case scenario, with 60% of the population getting the virus within six months, the country would require more than seven times the number of available hospital beds.
How Will It Affect Your Region?
Want to know how hospitals in your region would be affected in each scenario? You can check how your current location will be impacted by entering your city or zip code in the search bar featured in ProPublica’s report, or you can enter a different location to view its predictions.
The search provides an estimate of how many people over the age of 18 would be infected in the various scenarios, along with how many beds the region would need to treat those infected. It also shows which communities could be under capacity and have the most number of free beds available.
“Our model gives hospital leaders and policymakers a clear sense of when they will hit capacity and strategic information on how to prepare for rising numbers of patients,” Jha said. “If people wonder ‘Why am I social distancing?’ and ‘Why am I isolating myself?’ this data makes that real. People should look at this data and make sure their community has a plan.”







