This article, originally posted on Sept. 23, 2019, was last updated on Dec. 3, 2025.
Please note that these statistics aren’t updated regularly. Always check with your state’s hospital associations for the most up-to-date information.
Hospitals often use color codes to alert staff to an emergency or another significant event. These emergency codes allow trained hospital personnel to respond quickly and appropriately to various incidents.
Hospital emergency codes have often varied widely by location — even within hospitals in the exact same community — often leading to confusion. In 2023, anonymous electronic surveys asked 304 employees at five Georgia healthcare facilities to identify the codes for 14 different emergencies. On average, participants could correctly identify emergency codes just 44% of the time. Many participants reported that codes were only introduced at their orientation and were not practiced regularly.
“The results of our study suggest a prompt response to such incidents is likely to be poor, as most employees were unaware of the meanings or actions of these notifications,” co-author Morgan Taylor wrote in a news release.
This potential for confusion has led many states to adopt standardized codes for all hospitals.
In 2000, the Hospital Association of Southern California (HASC) released a handbook, “Healthcare Emergency Codes: A Guide for Code Standardization,” strongly urging a uniform code system after three people were killed in a shooting incident after the wrong emergency code was called. Code Gray, which typically means a combative person, was announced, drawing staff members toward the shooter. At the time of this incident, in California hospitals, 47 different codes were used for infant abduction and 61 were used for a combative person.
Three years later, Maryland mandated that all acute hospitals in the state have uniform codes. In fact, Maryland is the only state to mandate that hospitals implement uniform code terminology, requiring the adoption of a standard color code system as a component of emergency disaster plans. Maryland’s uniform emergency codes date back to 2002 and include:
- Code Red: Fire
- Code Pink: Infant or child abduction
- Code Blue: Cardiac or respiratory arrest
- Code Green: Combative person
- Code Gold: Bomb threat
- Code Orange: Hazardous material spill or release
- Code Gray: Elopement
- Code Purple: Security-only response
- Code Yellow: Emergency or disaster
- Code Silver: Active shooter
According to a January 2020 report from the Iroquois Healthcare Association (IHA), other states that recommend color code standardization include Arizona, Colorado, Florida, Hawaii, Kansas, Kentucky, Louisiana, Maryland, New Hampshire, North Carolina, Ohio, Oregon, Rhode Island, West Virginia and Wisconsin.
When this article was originally published, six fewer states had recommended color code standardization, demonstrating the growing realization of its importance.
25 State Hospital Associations Recommend Plain Language Hospital Emergency Codes
In Jan. 2020, at least 25 state hospital associations had recommended plain language alerts, including Colorado, Florida, Iowa, Minnesota, Missouri, North Carolina, New Jersey, New York, Pennsylvania, South Carolina, Texas, and Wisconsin. Most recently, in Feb. 2025, the Washington State Hospital Association (WSHA) recommended standardized plain language overhead paging codes across Washington state hospitals to improve clarity and emergency response times.
Some health systems aren’t waiting for state hospital associations or state officials to tell them to switch to plain language. For instance, in 2019, Piedmont Healthcare adopted plain language alerts at its 11 hospitals in Georgia. Eric Bour, MD, CEO at Piedmont Newton Hospital in Covington, said there was overlap with some of the most commonly used codes and many facilities used codes that were unfamiliar to the health system employees and professionals traveling between hospitals, according to Relias Media.
“Within one facility, it wasn’t a big deal because people were trained to know their hospital’s particular codes,” he said. “But … there is a potential that someone in one facility would not respond correctly to an event because they would not know what that particular color meant in that facility.”
Bour gave the example of Code Pink, a legacy color code that typically means infant abduction but can also mean an infant cardiorespiratory arrest.
“In one event, you want the place locked down and everyone doing everything you can to find that infant,” he said. “If it’s an infant cardiac arrest, you want the code team, and failure to respond appropriately in either case could be disastrous.”
Other healthcare worker organizations that recommend the use of plain language for hospital emergencies include more than a dozen different state hospital associations, patient safety organizations, and healthcare worker organizations, including the Emergency Nurses Association (ENA), the American Hospital Association, the Federal Emergency Management Agency (FEMA), the U.S. Department of Homeland Security (DHS), the National Incident Management System (NIMS), the Institute of Medicine, the Joint Commission, Centers for Disease Control and Prevention (CDC), the Food and Drug Administration (FDA), Centers for Medicare and Medicaid Services, and U.S. Department of Health and Human Services.
It is important to note that while there is significant agreement among the 10 color code systems we’ll address in this article, there is no national standard for emergency color codes, leading to inconsistencies among standard systems that are used by each state. This is demonstrated in the chart below from IHA’s report.
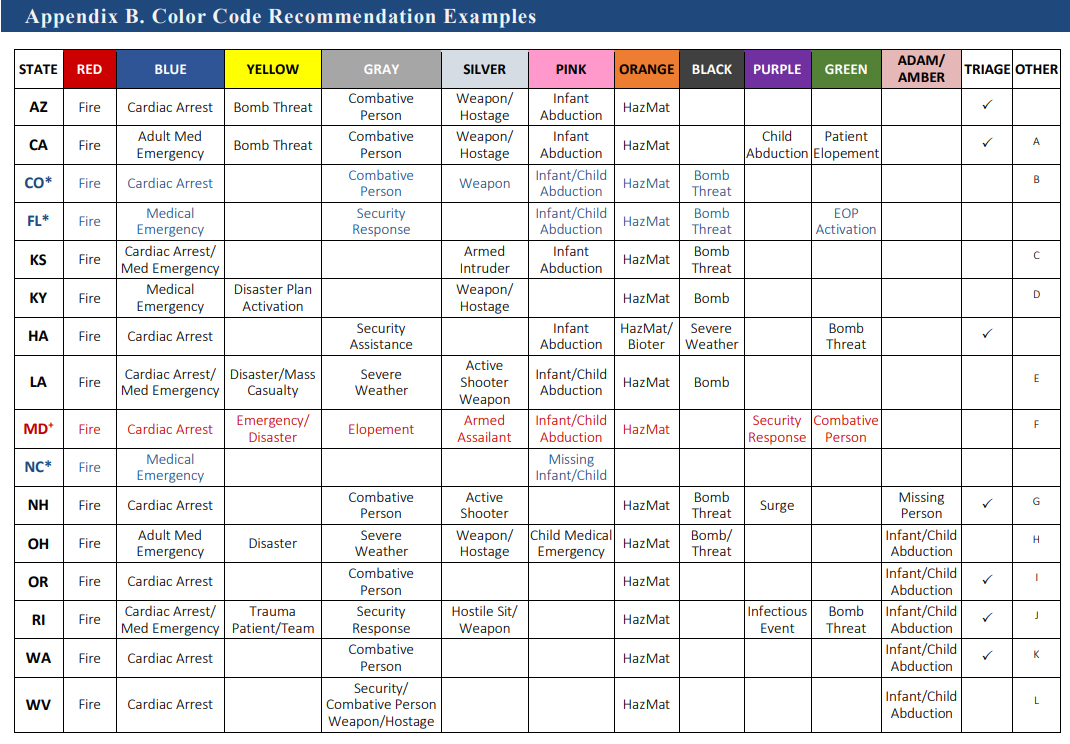
(Graphic: Hospital Emergency Codes Standardization and Plain Language Recommendations and Guidance, Iroquois Healthcare Association)
Code Blue
Code Blue means someone is experiencing a life-threatening medical emergency, typically an adult. It often means cardiac arrest or respiratory failure. All staff members near the location of the code may need to go to the patient. Most of the time, each employee has a preassigned role in the event of a Code Blue.
Code White
Code White indicates a baby or child is experiencing a life-threatening medical emergency. Having a different code for a pediatric emergency is important since treating children often requires specialized equipment.
Code Red
Code Red alerts hospital staff to a fire or probable fire. A Code Red may also be activated if someone smells or sees smoke. This code will often come with information about the fire’s location and will typically require evacuation.
Code Purple
Code Purple means a missing child or child abduction. In most cases, the hospital will go on lockdown during the search for the child to ensure no one leaves the building with them. The code is often accompanied by additional information, including what they were wearing, where they were last seen, who they were last seen with, etc.
Code Pink
Code Pink is similar to Code Purple but denotes an infant abduction.
Code Gray
Code Gray indicates a combative or aggressive person, requiring security personnel. It is also typically accompanied by a description of the dangerous person(s) and their location.
Code Orange
Code Orange can vary. While it also denotes a combative or aggressive person at some hospitals, at most, it means a call for medical decontamination, typically due to a hazardous fluids spill, like chemicals or patient blood.
Code Green
Code Green seems to be the most wavering code, but overall, it indicates the hospital is activating an emergency operations plan. Some hospitals use it to alert the arrival of patients from a mass casualty event while others use it to denote a missing high-risk patient. Typically, the code announcement also includes which emergency operations plan should be activated.
Code Silver
Code Silver alerts hospital staff to a person with a weapon and/or active shooter and/or hostage situation. Be sure not to confuse this with a Silver Alert, which some cities, including New York, use when there are missing seniors in imminent danger due to severe cognitive impairments or urgent need of medical care.
Code Black
Code Black indicates a bomb threat. Each hospital should have an evacuation protocol in the event of a bomb threat.
Uniform Hospital Emergency Codes Used in All Ontario Hospitals
While inconsistent hospital emergency codes is by no means an issue unique to the U.S., other parts of the world have been using common sense uniform emergency codes for years. Martin Green, now principal consultant for Martin Green & Associates, was working healthcare security at St. Joseph’s Healthcare System in Toronto in 1985. Quickly becoming involved in emergency planning and procedures, Green noticed emergency codes used at the hospitals were all formatted differently. For example, a fire alarm was announced as “Doctor Red,” a cardiac arrest was a “Code Blue,” and a violent situation was “Code 710.”
Green took it upon himself to reach out to all hospitals in Toronto to voice his concerns. Although met with much hesitancy and adversity, Green eventually teamed up with James Hanna, a well-known emergency management consultant, to create uniform hospital emergency codes.
Hanna came up with the idea to link the code with a specific color that added relevance to the code, making it easier to remember. Those codes are as follows:
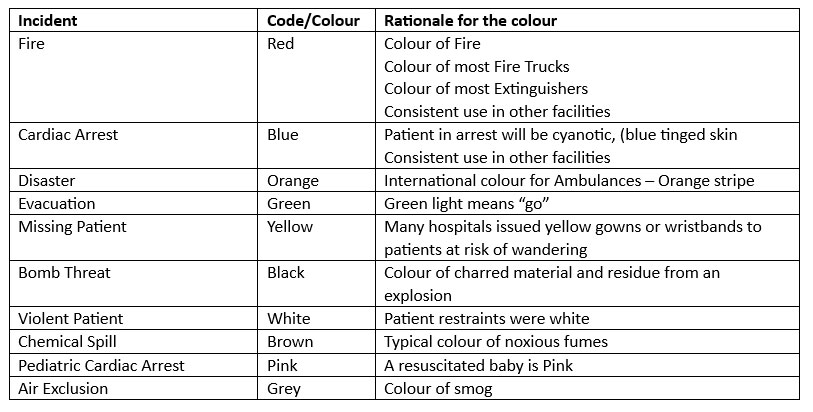
Hanna presented the final results to the Ontario Hospital Association, which ultimately led to the codes being adopted in every hospital and healthcare facility in Ontario.

